The Importance of Pressure Area Care
Introduction:
Pressure area care, is a critical aspect of nursing practice aimed at preventing skin breakdown and promoting optimal patient comfort. In healthcare settings, patients with limited mobility or prolonged bedrest are particularly susceptible to developing pressure injuries, making diligent prevention and management strategies essential.
This blog explores the significance of pressure area care in nursing, highlighting best practices, prevention strategies, and the impact on patient outcomes.
Understanding Pressure Injuries:
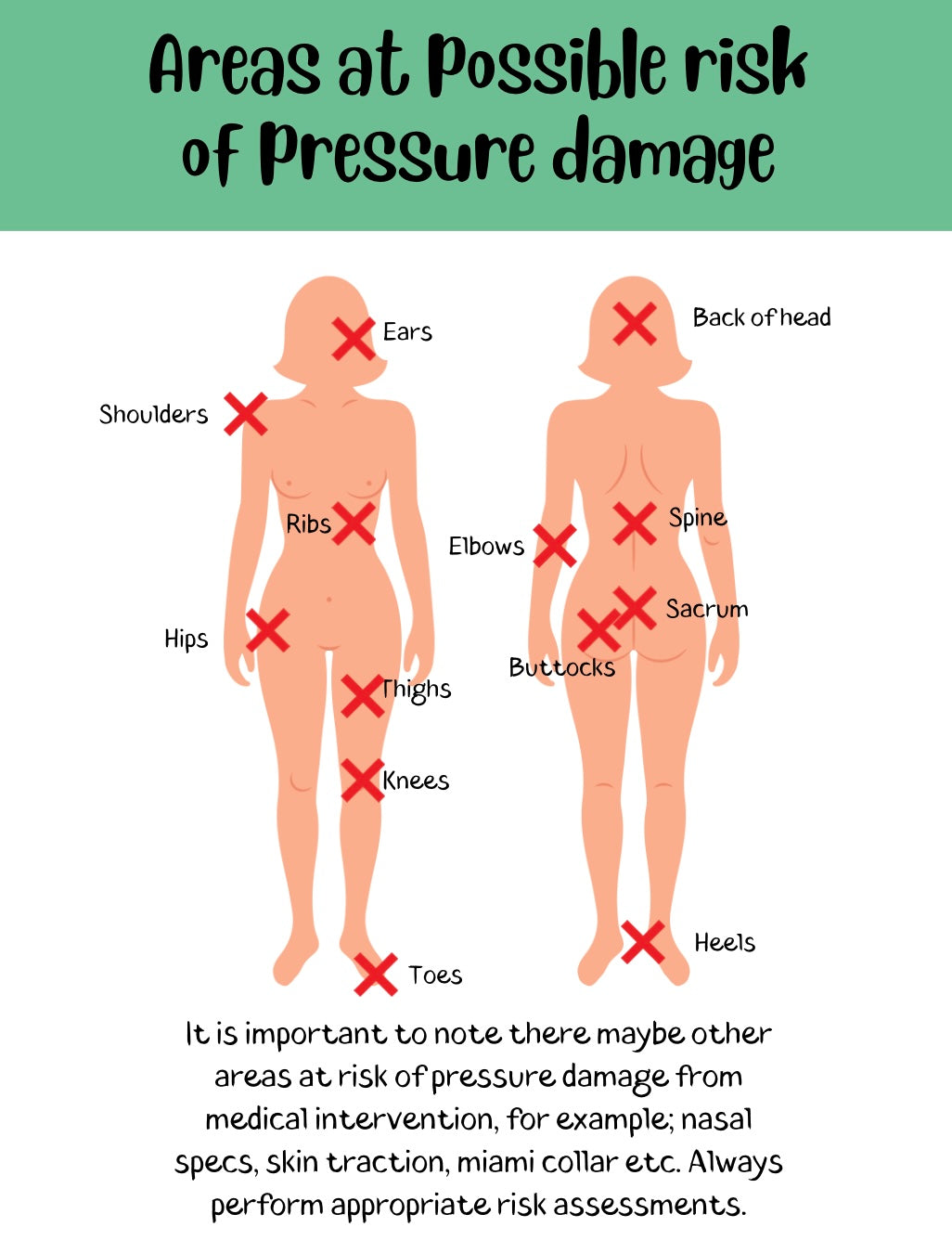
Pressure injuries, also referred to as pressure ulcers or bedsores, develop when prolonged pressure or friction on the skin reduces blood flow to the affected area, leading to tissue damage. Common sites for pressure injuries include bony prominences such as the heels, sacrum, hips, and elbows. These wounds can range from mild redness or skin irritation to deep, open sores that expose underlying tissues and increase the risk of infection.
The Role of Nurses:
Nurses play a pivotal role in preventing pressure injuries and managing existing wounds through comprehensive assessment, proactive interventions, and ongoing monitoring. By implementing evidence-based guidelines and individualised care plans, nurses can mitigate risk factors, promote skin integrity, and optimise patient comfort. Furthermore, nurses serve as educators, empowering patients and caregivers to participate in pressure area care and recognise early signs of skin breakdown.
Key Components of Pressure Area Care:
Effective pressure area care involves a multidisciplinary approach and encompasses several key components:
1. Skin Assessment: Regular skin assessments are essential for identifying areas of concern, assessing tissue viability, and documenting changes in skin integrity. Tools such as the Braden Scale are usual to assess risk factors and tailor interventions accordingly.
2. Pressure Redistribution: To alleviate pressure on vulnerable areas, health care staff can employ various measures such as repositioning techniques, turn charts, specialty support surfaces (e.g., pressure-relieving mattresses, cushions), and assistive devices to maintain proper alignment and reduce friction.
3. Skin Hygiene: Maintaining clean, moisturised skin is essential for preventing skin breakdown. Health care staff can educate patients on proper hygiene practices, including gentle cleansing, moisturising, and avoiding harsh chemicals or excessive moisture.
4. Nutrition and Hydration: Adequate nutrition and hydration are crucial for supporting skin integrity and promoting wound healing. It’s important tocollaborate with dietitians and healthcare providers to ensure patients receive appropriate dietary interventions and nutritional supplementation as needed.
5. Education and Empowerment: Patient and caregiver education is paramount in preventing pressure injuries and promoting self-care practices. Health care staff provide instructions on skin inspection, pressure relief techniques, nutrition, and the importance of regular movement and positioning.
To learn more about pressure sores and the stages you could grab the little book of Nursing Notes linked below.